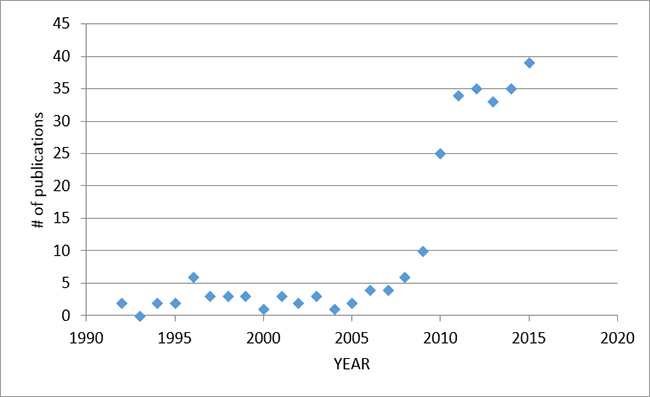
In 2015, there were 39 publications on PUBMED, including 24 original scientific papers, 4 case reports, 3 editorials, and 8 reviews.
Les études chez les adultes
24-hrs evaluation of patient-ventilator interaction during NAVA vs. PSV
In 30 difficult to wean adult patients (mean duration of ventilation 33 days), Younis et al (BMC Anesthesiology) collected ventilator and physiological data over two 23-hr periods (either during NAVA or PSV), followed by a cross-over to the other mode. 80% of the patients underwent the PSV mode first. They found a lower total number of asynchronies and lower asynchrony index in the NAVA mode, as well as increased variability of tidal volume and oxygenation parameters.
Ce manuscrit a été accompagné d'un éditorial de Kacmarek et al (BMC Anesthesiology), Qui a suggéré que, dans la plupart des cas, il convient d'utiliser les modes d'attribution proportionnelle.
Neurally déclenché par l'appui de la pression chez les patients atteints de BPCO
Utiliser le ventilateur Servoi mis en mode NAVA avec le niveau le plus élevé possible de NAVA, Liu et al (Soin critique) Utilisé des ajustements dans les limites de pression supérieure pour imiter le soutien de pression neurale déclenché (PSN). A différents niveaux de PEEP, ils ont comparé l'interaction patient-ventilateur et les variables physiologiques au cours PSN et pendant l'appui de pression à commande pneumatique (PSP) Chez 12 patients atteints de BPCO avec PEP intrinsèque connue. L'indice de asynchronisme était plus faible avec le PSN par rapport au PSP, Et est resté faible avec PSN, Même à zéro PEEP. L'impact de la synchronie amélioré a été réduit de pré-déclenchement et les efforts mécaniques inspiratoire (évalués par ballonnet oesophagien). Pendant PSP fixé à "PEEP optimal" (PEEP réglé à 80% de PEP intrinsèque), l'effort de déclenchement a été réduit au cours de PSN, Même lorsque BEEP était de zéro. Les auteurs ont conclu que PSN supprime la nécessité d'une PEEP extrinsèque chez les patients atteints de BPCO (dans le but de déclencher l'effort).
Pression Lung-distendre pendant NAVA dans le SDRA
Doorduin et al (Critical Care Medicine) studied 12 patients with mild to moderate ARDS while breathing with three different ventilation modes (Pressure Control (PCV), Pressure support (PSV), or NAVA). The aim was to compare tidal volume and lung-distending pressure (transpulmonary pressure) between modes. The authors found that as patients were given more “freedom” to control the level of assist (PCV to PSV to NAVA), they were able to maintain lung protective ventilation with NAVA (mean chosen VT ~6.0 ml/kg), with the added benefits of improved respiratory variability and improved patient-ventilator interaction.
Patient vs. Ventilator Contribution to Tidal Volume
In an attempt to reproduce the PVBC concept in humans (“patient-ventilator bReath contribution” index, Grasselli et al 2012 ICM), Liu et al (Soin critique) studied 12 intubated patients with acute respiratory failure during NAVA ventilation at different NAVA levels. At each NAVA level, for one breath, the assist was removed. The authors then calculated a ratio of tidal volume per Edi (VTinsp/Edipk) for this non-assisted breath, as well as for the preceding assisted breath(s). By dividing the Vtinsp/Edipk of the unassisted breath by the same ratio of the assisted breath, it was shown that this PVBC index was correlated to the gold standard index of esophageal pressure to transpulmonary pressure (Pes/PL). Squaring the PVBC increased this correlation to Pes/PL. Even further improvements were found if the average of five assisted breaths was used in the calculation of PVBC, and if the Edipk values were reproducible (30% error acceptable).
NAVA vs. PAV
En Soin critique, Schmidt et al compared PSV to two modes of proportional assist, NAVA and proportional assist ventilation (PAV), in 16 intubated patients (mainly ARDS and pneumonia). The main physiological outcomes included ventilation variables (and their variability), Edi, blood gases, and patient-ventilator asynchronies. The intervention was three different levels of support (initial 6-8 ml/kg, 50% lower, and 50% higher assist). The authors found better patient-ventilator interaction with PAV and NAVA, as well as improved variability in tidal volume. The only significant differences between PAV and NAVA were better proportionality with NAVA, and more double triggering (albeit a small frequency of these events per minute). Compared to PSV, both NAVA and PAV limited over-distension when the assist was increased.
Modélisation mathématique des voies respiratoires élastance pendant NAVA et le PSV
Dans un PLoS ONE article, Chiew et ses collègues a obtenu des données expérimentales chez 22 patients pour valider un modèle de élastance variant dans le temps chez les patients respirant spontanément, en utilisant deux modes, NAVA et le PSV. élastance (EDRS) trajectoires variables dans le temps ont été cartographiées et jugés significativement différente entre les deux modes. Une valeur EDRS positive est à prévoir pour les patients qui ne sont pas spontanément à respirer (pleine aider), tandis qu'une valeur négative EDRS est indicative d'une contribution plus importante de l'effort patient (pression pleurale plus négative).
Diaphragme à ultrasons et Edi en Mécaniquement patients ventilés
Goligher et al, dans une étude unique (ICM), investigated the feasibility, reproducibility, and validity of measuring diaphragm thickness with ultrasound in mechanically ventilated patients. In 96 patients on mechanical ventilation, and in 9 healthy subjects (breathing spontaneously with different maneuvers), diaphragm thickening (an indication of inspiratory effort) and diaphragm thickness (an indication of diaphragm atrophy) were measured and compared to Edi. Right hemi-diaphragm thickness measures were highly reproducible, whereas diaphragm thickening fraction was only moderately reproducible, but was correlated to Edi. Patients who had undergone mechanical ventilation with neuromuscular blockade had a lower inspiratory thickening fraction, compared to those patients who received only partial ventilator assist, and healthy subjects.
Respiratory Muscle Unloading during NAVA vs. PSV
In 11 adult patients recovering from acute respiratory failure, Carteaux et al (Crit Care Med) sought to find comparable levels of respiratory muscle unloading during PSV and NAVA. In a randomized fashion, patients were studied at nine different NAVA levels, and at five different PSV levels, and indices of muscle unloading were calculated at each. More specifically, to express the percentage of assistance in a comparable way between the two modes, the authors calculated a ratio to quantify the proportion of the total pressure that was assumed by the ventilator (the remainder being the patient’s contribution). They concluded that – in terms of respiratory muscle unloading – levels of NAVA between 0.5 and 2.5 cm H2O/uV were comparable to PS levels ranging from 7 to 25 Cm H2O.
Volume Tidal pendant NAVA Ventilation après Double Lung Transplant
Dans une lettre à l'éditeur du American Journal of Respiratory and Critical Care Medicine, Rozé et al report in a group of post lung-transplant patients (n = 14 ) the spontaneously chosen tidal volume while breathing on NAVA. A group of non-transplanted patients (surgical patients failing routine SBTs) served as controls. The transplanted patients demonstrated tidal volumes ranging from 2.9-7.5 ml/kg (mean 5.3 ml/kg). When hypercapnia was considered, there was no difference in tidal volume: 4.8 (1.2) ml/kg in the hypercapnic group vs. 5.9 (1.2) ml/kg in the non-hypercapnic patients. The tidal volume in the control group was 6.5 (1.5) ml/kg and was significantly higher than in the transplanted patients. This is the first study to demonstrate that bilateral vagal denervation is not an exclusion for NAVA ventilation, in terms of the spontaneously chosen tidal volume.
Économies potentielles avec NAVA chez les adultes
Hjelmgren et al (Les progrès thérapeutiques dans Resp Dis) conducted an economic evaluation of NAVA compared with PSV based on previous reports showing an indirect link between improved patient-ventilator synchrony and time on ventilation. The cost of Swedish ICU cost and NAVA costs were incorporated into the model. The authors found a 31% improvement in synchrony with NAVA for all studies published, and extrapolated a 1.7 days reduction in days on mechanical ventilation. This would theoretically correspond to a cost savings of US$ 7886.
Les études chez les enfants
Surveillance Edi cours haut débit Canule nasale chez les nourrissons prématurés
Regarding Edi monitoring during nasal HFNC, Nasef et al (Acta Pediatr) compared neural breathing pattern during nasal CPAP and nasal HFNC matched to target the same mean airway pressure, in ten preterm infants (<1500 g). They found that nasal HFNC was associated with higher Edi peak, and increased neural inspiratory time, compared to nasal CPAP. As well, they observed a discrepancy between the respiratory rate of the patient determined from the Edi, and the respiratory rate noted by readings from the plethysmograph.
NIV-NAVA Améliore patient-Ventilator Interaction chez les enfants
In a physiological cross-over study by Ducharme-Crevier (Crit Care), NIV-NAVA was compared to conventional NIV (CPAP, PSV, or PCV), in 13 children admitted to the PICU for respiratory failure (interquartile age range 2-109 months), eight of which had pneumonia or bronchiolitis. The authors found that during conventional NIV, patients spent between 27-32 percent of the time in asynchrony, while it was only 8% of the time in NIV-NAVA. This was mainly a result of reduced trigger delay, reduced cycling-off delay and less ineffective efforts.
NIV-NAVA Améliore patient-Ventilator Interaction dans Preterm Neonates
The group of Lee et al (Arche Dis Child Fetal Neonatal Ed) examined timing errors between the Edi and ventilator pressure in 15 premature infants (mean GA 27 weeks) during NIV-NAVA and NIV-PSV. Besides a reduced amount of ineffective efforts and reduced auto-triggering, the authors found shorter trigger delays, and shorter time “in excess” during NIV-NAVA compared to NIV-PSV. During NIV-NAVA, the Edi and peak inspiratory pressure were lower. The overall asynchrony index during NIV-PSV was 74% (compared to NIV-NAVA 20%).
Utilisation de NAVA dans Nordic réanimation pédiatrique pour le traitement de lésion pulmonaire aiguë
This study by Jensen et al (Acta Anesthesiol Scand) used questionnaire responses from 18 large Nordic ICUs that treat children with ARDS. NAVA was used in 44% of the units. They also found that other ventilation treatment strategies (cuffed endotracheal tubes, use of ECMO, etc…) for pediatric ARDS in the Nordic countries are relatively uniform and largely in accordance with international practice.
L'effet de la caféine du Neural respiratoire Entraînement
In 17 premature infants on various modes of ventilation, the Edi waveform was analyzed before and after administration of a loading dose of caffeine citrate. Parikka et al (Early Human Dev) demonstrated a reduced number of central apneas (5-10s), and increased Edi amplitude after caffeine.
Tonic Edi avec et sans aider à l'USIP
In 52 children (median 10 months old; inter-quartile range 1-49 months), Edi was recorded for 1-hour intervals at four periods throughout the PICU stay (acute phase, pre-extubation phase, post extubation phase, and at PICU discharge). The authors quantified the tonic Edi, and found in children <1 yr old (n=28), that tonic Edi increased from the acute phase to PICU discharge, but because inspiratory Edi concomitantly increased, the Edi as a percentage of the inspiratory effort, actually diminué over the course of PICU stay. In most of the older patients, tonic Edi was negligible (<0.5 uV), but could exceed over 1 uV at some point during the stay, indicating that older children can exhibit some degree of tonic Edi. Bronchiolitis was the only independent variable associated significantly with tonic Edi.
Impact de Sédation sur Edi dans l'USIP
In the PICU, 20 children weaning from analgesia and sedatives were included and Edi was measured. The intervention in this study by Amigoni et al ( ICM) was a bolus of propofol (1 mg/kg), and the outcome was the Edi waveform’s lowest value (and time to reach that value). The mean decrement in Edi was 32%, most patients requiring less than 2 minutes to reach the lowest Edi. Backup ventilation had to be initiated in 6 children after a mean time of 6 minutes from drug administration. The authors concluded that the Edi signals should be used to measure the degree of respiratory depression, in order to better titrate the dosage.
Reflex Down-règlement de Edi avec des niveaux croissants NAVA dans Neonates
In agreement with studies in adult patients and in animals, Firestone et al (Journal of Perinatology) demonstrated an appropriate reflex response (i.e. down-regulation of Edi) to increasing NAVA levels in 21 preterm newborns (9 with invasive NAVA, 12 with NIV-NAVA). In the NAVA group, the mean birth weight was 703 g (380-960g) and in the NIV-NAVA group, it was 835 g (490-1060 g). In both groups, the NAVA level was initially set to 0.5 cm H2 O/uV, and was then increased in steps of 0.5 every 3 min until a NAVA level of 4 cm H2O / uV. Dans un premier temps, la pression inspiratoire de pointe augmente avec les niveaux NAVA, mais a atteint un "point de rupture" (BRP), où il n'y a plus augmenté, en dépit de l'augmentation des niveaux NAVA. Ceci est dû à la régulation négative de l'EDI (jusqu'à 53% à la BrP). Le volume courant également "atteint un plateau" au BrP.
NIV-NAVA chez les enfants après chirurgie cardiaque
Chez les enfants plus jeunes recevant NIV d'une assistance respiratoire après chirurgie cardiaque, Hoetekie et al (Respiratory Care) performed a cross-over study by randomizing babies (age range 1-22 weeks, and less than 5 kg) to either nasal CPAP or NIV-NAVA right after extubation. The peak Edi values during NIV-NAVA were significantly lower during NIV-NAVA, indicating more diaphragm unloading compared to nasal CPAP. Synchrony analysis was reported for NIV-NAVA, and showed (despite average leakage of 70%), 99% neural triggering (compared to 95% in the Vignaux (5) study), with a low inspiratory trigger delay.
NAVA et gain de poids en très faible poids à la naissance Nourrissons
dans le Journal of Clinical Néonatologie, RAHMANI et al. effectué une analyse rétrospective des dossiers médicaux et a trouvé le gain de poids médian pour les bébés qui ont été traités avec NAVA était plus élevée (30g / jour) que la ventilation conventionnelle (13 g / jour), malgré le même apport calorique moyen. Les auteurs ont proposé un modèle pour prédire les économies de coûts et une réduction LOS. Ils ont conclu que cette étude est la première à donner un aperçu de l'impact financier potentiel de mise en œuvre de NAVA.
NAVA Avant et après l'extubation chez les nourrissons à terme
Longhini et al (Minerva Pediatric) Ont analysé les variables physiologiques et ventilateur en 10 nourrissons nés à terme (poids moyen 3 kg) de respiration pendant 2 heures tandis que intubé sur NAVA puis extubation à NIV-NAVA, avec les mêmes réglages du ventilateur. Les auteurs ont constaté aucune différence en termes d'échange de gaz ou d'un motif de respiration entre les deux périodes de ventilation. Fait à noter, il n'y avait aucune différence dans l'interaction patient-ventilateur, les exigences de sédation, ni les signes vitaux pour invasifs ou NIV-NAVA.
animal Studies
Neurally Ajusté PEEP chez les animaux
Chez les lapins confrontés à des défis respiratoires (résistance, réinhalation de CO2, et une lésion pulmonaire aiguë), Liu et al (BMC Anesthesiol) described for the first time the concept of “Continuous NAVA” (cNAVA). cNAVA is a new respiratory support device where the Edi controls the delivery of assist continuously both during inspiration and during expiration. (This is different from the commercially available mode known as NAVA which is triggered and cycled-off by the Edi, and is limited to proportional assist on inspiration only, with a fixed PEEP). With cNAVA, if there is Edi during exhalation (“tonic Edi”), assist will be delivered in proportion, hence a “neurally adjusted PEEP”.
Les rapports de cas
In 2015, case reports were published demonstrating the clinical use of Edi monitoring and NAVA in an adult patient with tetanus (Tane, Respiratory Care), in neonates undergoing treatment with albuterol (Snow, Advances in Neonatal Care), and in two children with pulmonary interstitial edema (Lee, Journal of Clinical neonatology). One article reported the misplacement of the NAVA catheter into the lung (van Kerckhoven), the latter which can be avoided if the appropriate steps are taken for catheter insertion and placement.
