Post 1: Proportionality and NAVA level
Patient ventilator interaction has generally two dimensions: timing of assist (temporal interaction) and magnitude of assist (interaction in space), both in relation to patients effort. Temporal interaction relates to synchronization of assist delivery to inspiratory effort (i.e. ideally a simultaneous start and termination of inspiratory effort and assist). Interaction in space relates to synchronization of patient inspiratory effort to magnitude of ventilator assist (i.e. proportionality between inspiratory effort and magnitude of assist). The ability to allow spatial interaction between the patient-and-ventilator is what fundamentally defines modes like NAVA and PAV (Proportional assist ventilation) and differentiates them from conventional pressure and volume targeted modes.
Proportionality stands for – relationship of two variables whose ratio is constant. The NAVA level is a proportionality constant used to adjust the pressure delivered from the ventilator to be proportional to EAdi. EAdi represents neural respiratory drive to the diaphragm- see Post 3 on Diaphragm Electrical Activity.
During ventilation with NAVA, the magnitude of inspiratory pressure assist will always vary to match changes in the magnitude of neural inspiratory drive. Consequently, the inspiratory pressure waveform of the ventilator should resemble the EAdi waveform, which in fact means that every increase in neural inspiratory effort of the patient is rewarded by a proportional increase in pressure assist. Also, consider that the EAdi signal regulates inspiratory muscle activation and generates lung distending pressure. The result during NAVA is that the patient’s inspiratory muscles induce a negative pressure deflection around the lungs (measured as pleural or esophageal pressure) and the ventilator generates a positive pressure deflection into the lungs (measured as airway pressure), esophageal pressure waveform being a mirror image of the airway pressure waveform. NAVA thus can be considered to act as an extra inspiratory muscle under the same neural control as the in situ respiratory muscles, sharing the work to maintain alveolar ventilation.
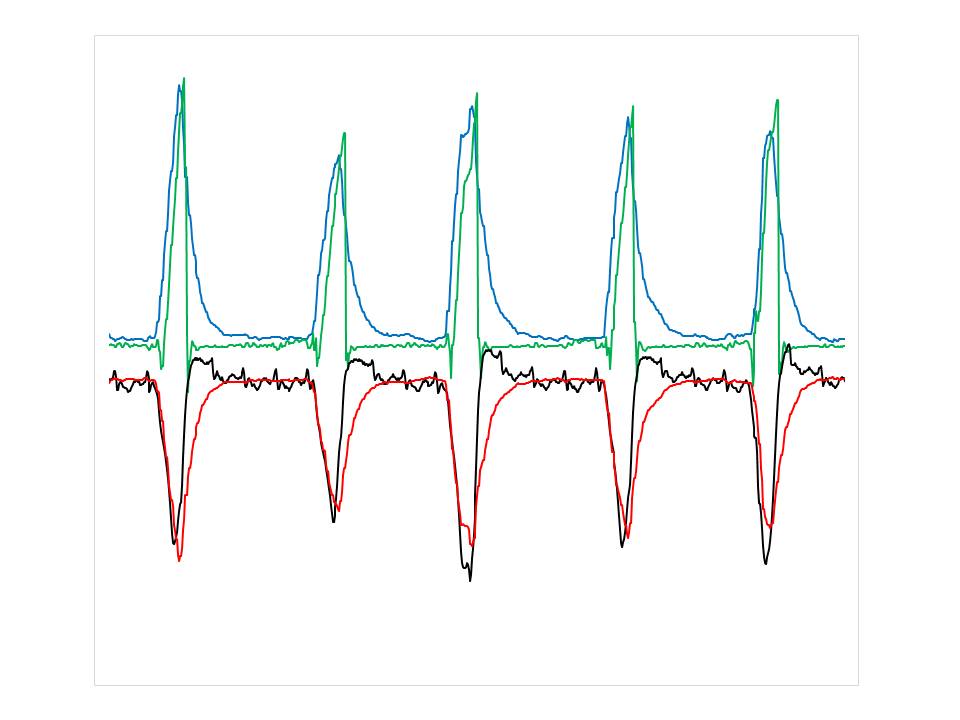
Figure shows five assisted breaths in a patient on NAVA, green line shows airway pressure, black line shows esophageal pressure, blue line shows EAdi superimposed to airway pressure, red line shows the same EAdi signal reversed and rescaled in amplitude to superimpose over esophageal pressure. First, observe the close resemblance of inspiratory wave forms for esophageal pressure (black line) and “mirrored” EAdi (red line). Second, observe close resemblance of inspiratory pressure assist (green line) and EAdi (blue line). This shows that the neural control of assist ensures its delivery in synchrony to inspiratory effort, most importantly the patient controls (via the EAdi blue and red lines) both his own lungdistending pressure (black line) as well as that delivered by the ventilator.
The NAVA level determines the ratio of pressure delivered for a given EAdi and thus the contribution of pressure from the ventilator – the higher the NAVA level the higher the pressure for a given EAdi. We showed in our early studies that increases in NAVA level reduced the inspiratory esophageal pressure swings which is indicative of respiratory muscle unloading. At the highest NAVA levels used, it was possible to abolish or even reverse the inspiratory esophageal pressure swings such that the respiratory muscles were not at all contributing to inspiration. In other words, high NAVA levels can eliminate work of breathing.
The NAVA level thus becomes the divider that can be used to control the patient’s contribution to work of breathing. In other words, the partitioning of total lungdistending pressure (trans-pulmonary pressure) i.e. the total pressure generated by the patient (esophageal pressure) and the ventilator (airway pressure) during an inspiration, is controlled by adjusting the NAVA level.
The units of the NAVA level is cmH2O/µV, which is in the same units as the patient’s neuro-mechanical efficiency (NME) of the inspiratory muscles. NME represents the amount of force – which can be measured as the pressure generated by the inspiratory muscles to expand the lungs, in relation to the neural inspiratory activation – that can be measured via the EAdi. Similar to the NAVA level, the units of the NME is cmH2O/µV. The NAVA level and NME thus represents the ventilator’s and patients efficiency to create lungdistending pressure, respectively. A simple way to measure NME at the bedside is by measuring changes in airway pressure and EAdi during an inspiratory occlusion starting at end-expiration (See Forum: “Edi as it relates to trans-pulmonary pressures”).
As an example of the clinical relevance of NME, we recently showed that average NME in a group of patients that was successfully weaned had an NME of about 1.5 cmH2O/µV during their spontaneous breathing trial whereas NME was reduced to about 0.5 cmH2O/µV in the group of patients that failed the spontaneous breathing trial (Liu et al Crit Care 2012). Same study also showed that, during the spontaneous breathing trial, the successfully weaned patients had significantly higher tidal volume and lower EAdi compared to those who failed spontaneous breathing trial. Consider that patients who failed were weaker (i.e. 1/3 of the NME) and had higher EAdi and lower Vt compared to successfully weaned patients, they would need more assist to increase Vt and maintain a tolerable EAdi. In this case, applying a NAVA level of 1.0 cmH2O/µV, would increase the total NME of the failed SBT group to that of the successful weaning group, and provide 3 times more transpulmonary pressure (i.e. patient + NAVA) for any given EAdi to generate the tidal volume.
Hence NAVA supports the patient’s inspiratory muscle function while allowing the patient to control his breathing pattern.