Post 4: Esophageal vs. Surface EMG measurements
Introduction
Electrical activity (also referred to as the electromyogram – EMG) of respiratory muscles has been used for decades, to for example asses activation and fatigue. I have previously described the signal principles in Post 1 and Post 3. The methods to measure diaphragm EMG have involved trans-esophageal measurements as presented in Post 2 but also other methods using surface electrodes as well as inserted wires or concentric needle electrodes. Their use has been previously described in “Electrophysiologic Techniques for the Assessment of Respiratory Muscle Function” (ATS/ERS Statement on Respiratory Muscle Testing, Am J Respir Crit Care Med Vol 166. pp 548-557, 2002).
History
Early work describing EMG of the human intercostal muscles with surface electrodes was presented by Campbell in 1955. He summarized “The intercostals are thin muscles, almost entirely covered by other muscles. There is no movement or action which is known to cause them to contract while the other muscles close to them are inactive. They are, therefore, difficult to examine electromyographically in the intact human subject because of the limitations of both surface and needle electrode techniques.”
The earliest Pubmed citation of trans-esophageal EMG measurements in humans is by Petit, Milic-Emili and Delhez in 1959. This was followed in 1960 by Agostoni, Sant’Ambrogio and Del Portillo Carrasco showing the link between diaphragm EMG and force. These works indicated less problems of identifying the diaphragm signal with trans-esophageal EMG compared to surface electrodes.
According to Pubmed the search term “diaphragm EMG” presents 1682 publications, the publication rate peaked in 1993 with 74 publications that year. “Intercostal EMG” presents 709 publications. Diaphragm surface EMG shows 168 publications. “Diaphragm esophageal EMG” has 179 publications. “Diaphragm needle EMG” gives 72 hits.
Types of measurement
Trans-esophageal EMG
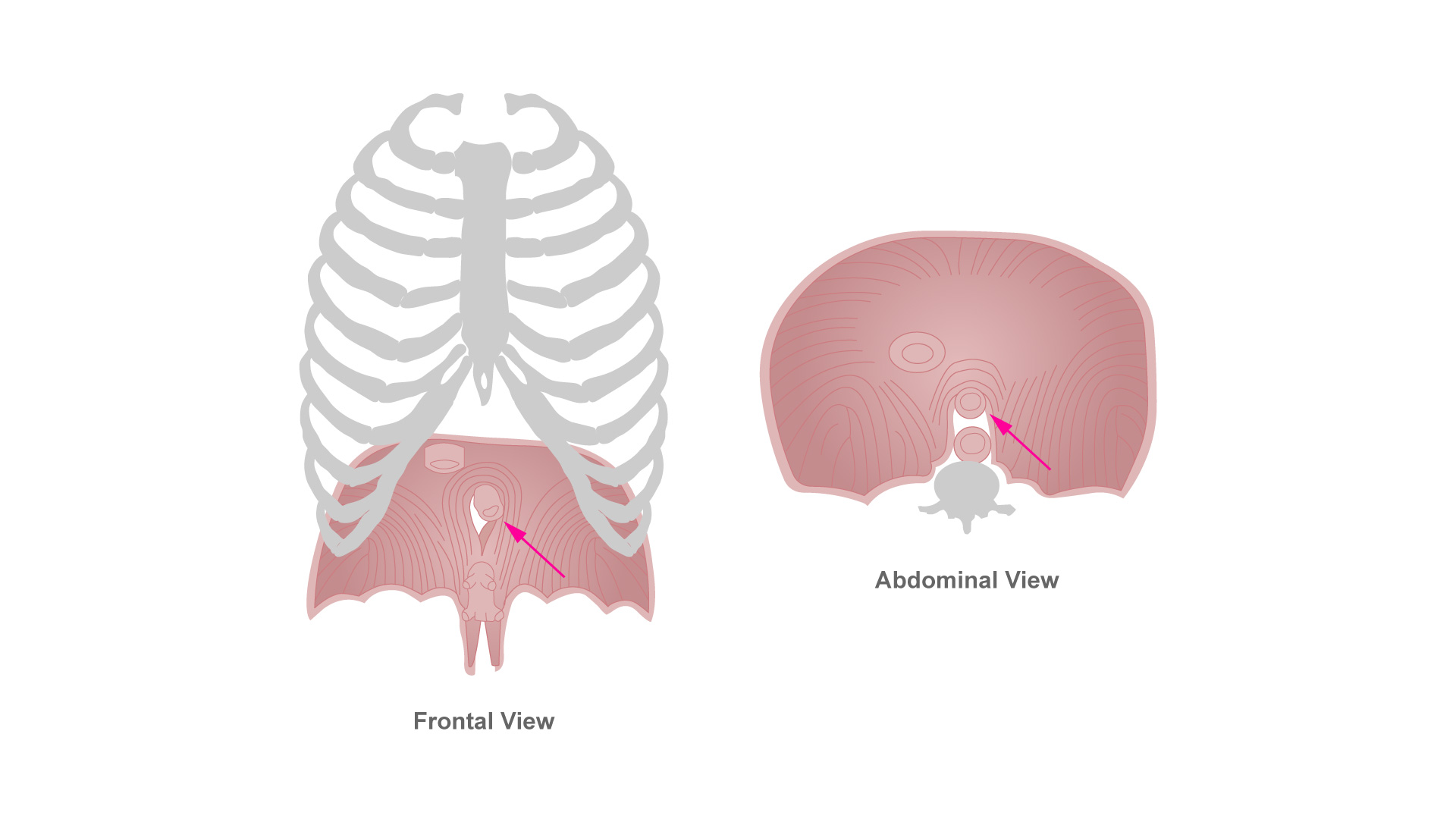
As the esophagus passes through the crus of the crural diaphragm frontal to the aorta, it is providing a measuring site far way from other inspiratory/expiratory muscles. Nonetheless one has to keep in mind that the esophagus is a muscle as well as the juxtaposed heart, both having several fold higher amplitude signals than the diaphragm, however characterized by a different frequency content (Sinderby et al 1995).
Surface EMG
Surface electrodes have been implemented on the lower ribcage to measure diaphragm EMG, over the intercostals to measure inspiratory and/or expiratory EMG, as well as over the accessory muscles. Typically two electrodes are attached to the skin over the region of interest to obtain one differential recording of respiratory muscle EMG. Depending on the site of interest, there are a different number of muscles involved in the EMG recording.
Diaphragm EMG is typically obtained with electrodes in the lowest inter-costal spaces in the midclavicular to midaxillary line. There are several layers of intercostal and abdominal muscles traversing this area which have inspiratory, expiratory and postural function. The diaphragm is the most distant muscle of all with regards to the electrodes.
- Parasternal muscles are recognized as inspiratory, however, they are covered by the pectoralis muscle.
- Accessory muscles are inspiratory and many, however, they are all fulfilling postural functions.
Needle and fine wire electrodes
Small electrodes with very small interelectrode distance can be used to obtain specific information form specific muscles when inserted into the muscle of interest. A problem is to know which muscle the electrode penetrates and to avoid pneumothorax. A recent solution to this problem is use of ultrasound (Amirjani et al 2012).
Cross-talk
Measurement of EMG is affected by cross-talk between adjacent muscles, that is similar to a microphone it is very difficult to get a selective recording of a specific muscle if adjacent muscles are active at the same time (Sinderby et al 1998). As an example consider the surface recording of the diaphragm. First breathing cannot be strenuous since this could involve inspiratory intercostals. Second if load or agony induces expiratory muscle activity of intercostal or abdominal muscles, this will also blend into the signal. Third, if patient is moving, postural activation of intercostal and abdominal muscles will induce tonic EMG activity. In other words, a standardized test situation for surface EMG measurements is crucial. Several groups have had successful use of surface EMG using standardized test situations – for example Reilly et al 2013, Duiverman 2004, Schmidt et al 2013, Maarsingh et al 2006.
Concentric needle and small wire EMG can be used to be more precise and avoid cross talk, however, these methods may be limited when it comes to global activation and long term measurements (Parthasarathy et al 2007, Butler & Gandevia 2008.)
Obesity
Increasing distance between the muscle (signal source) and the EMG electrodes reduces signal amplitude, mainly by loss of the signals high frequency components. Hence, at some point the signal-to-noise ratio will be too low to allow quality recordings. Obesity imposes a layer between the ribcage and skin surface, increasing muscle-to-surface electrode distance and impairing signal-to-noise ratio. To my experience, obesity does not appear to have a measurable dampening effect on trans-esophageal EMG recordings.
Conclusion
Concentric needle EMG can be used to measure specific motor unit activity. Specifically, the costal diaphragm activity can be successfully studied. Needle EMG is not affected by obesity and have little cross-talk from adjacent muscles.
Small wire electrodes, if placed with a small interelectrode distance, provides a more specific signal than surface electrodes and can be used to study motor unit actvity. EMG is not affected by obesity and have less cross-talk from adjacent muscles and the heart.
Surface electrodes provide EMG representative of global respiratory (i.e. inspiratory and/or expiratory) and postural muscle activity. The accuracy of the surface EMG method is highly depending on protocols implemented to standardize the measurement situation. To avoid cross-talk from adjacent muscles not associated with the activity of interest, e.g. EMG from pectoralis when trying to measurement EMG of the parasternals, it is important to control movement of the arms during recordings. To avoid that the muscle under study is activated for a reason other than that assumed by the investigator, e.g. postural EMG activity of intercostal muscles during study of EMG inspiratory activity, it is important that the upper body is carefully supported and body movements are avoided. EMG is affected by obesity and is strongly affected by cross talk from adjacent muscles including the heart.
Esophageal electrodes provide a global EMG (EAdi) activity of the crus of the crural diaphragm. This activity has been shown to relate to global inspiratory activation (Sinderby et al 1998, Beck et al 2001). Trans-esophageal EMG is not affected by obesity and has a well characterized cross-talk from the heart and esophagus that can be identified and handled.
Correctly protocolized, acquired, and analyzed, all methods for EMG measurements are valuable with regards to monitoring.
To control ventilatory assist, needle and fine wire electrodes may be limited because the measurements are very specific and can be difficult to maintain over time. EMG obtained by surface electrodes, is influenced by cross-talk, postural and expiratory muscle activity – the signal-to-noise ratio also being affected by obesity. As well electrodes may come loose when patients sweat or move. Transesophageal EMG (EAdi) , with a secured catheter, assuming adequate signal acquisition, processing, and management of electrode filtering and crosstalk from the heart and esophagus, has been found to reliably control ventilatory assist in patients of all ages (Sinderby & Beck, NAVA; in Principles and Practice of Mechanical Ventilation 3rd edition, ed. Tobin 2013).
For a recent update on EMG monitoring of respiratory muscles the interested is recommended to read Doorduin et al (2013).
