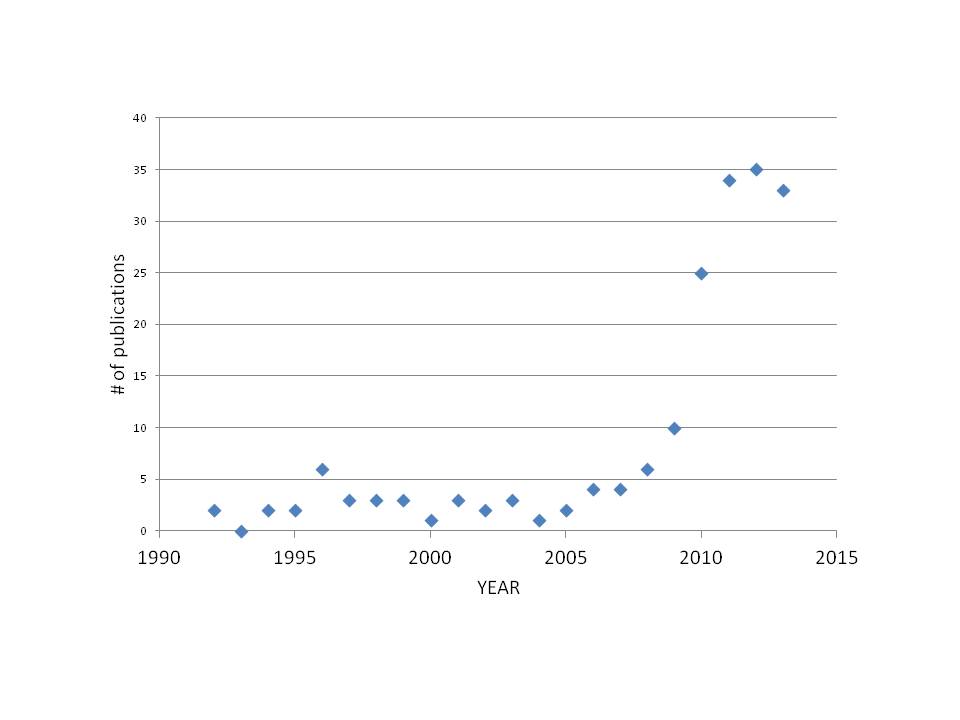
Happy 2014! May this year be filled with new science and improvements in mechanical ventilation! In 2013, nearly the same number of peer-reviewed papers were published (33 articles in PUB MED) compared to 2012 (35 articles).
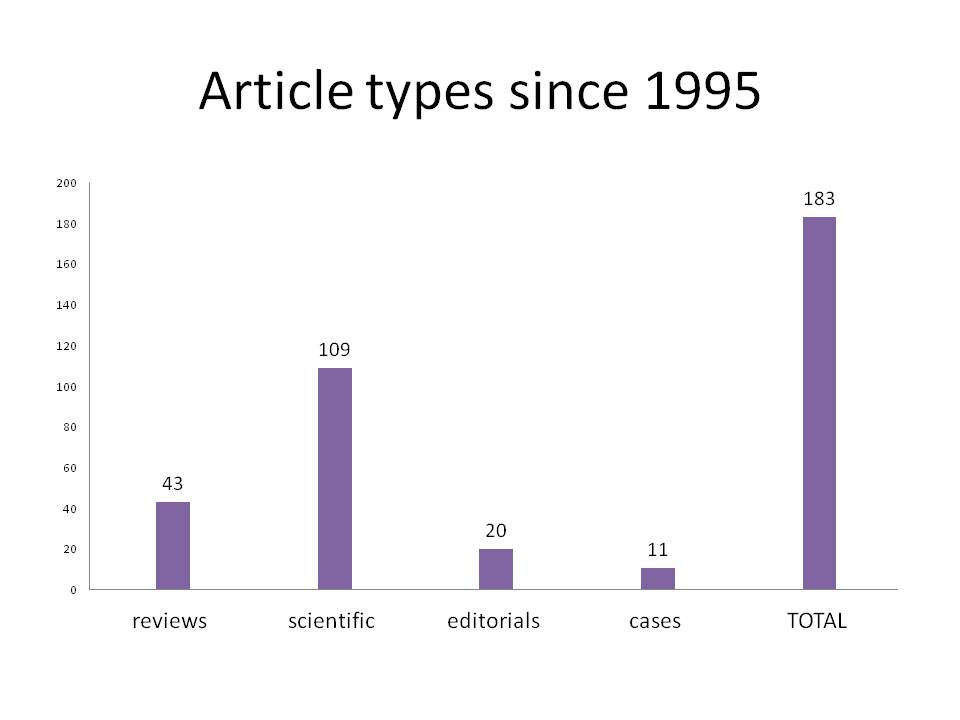
Over the last 20 years, the distribution of article “type” can be plotted as:
In 2013, the following articles were published:
Scientific papers (n= 13)
NAVA and sedation: Vaschetto et al, (CCM 2013), were the first to study the effects of sedation (Propofol) on patient-ventilator interaction during PSV and NAVA. In fourteen adult patients with ARF, they randomized 3 levels of PSV and 3 levels of NAVA, during wakefulness, light sedation and deep sedation. Reducing sedation caused an increase in (diaphragm electrical activity) Edi amplitude in both modes. Patient-ventilator interaction worsened (ineffective triggering) with increasing sedation in PSV, whereas with NAVA synchrony was present and not affected by sedation.
NAVA and ventilation distribution: Blankman et al, (ICM 2013) examined ventilation distribution (measured with EIT) at varying levels of PSV and NAVA in 10 adult patients with acute lung injury. Their results demonstrated higher aeration of the dependent lung regions during NAVA and less over-assistance compared to PSV.
Edi and work of breathing: Bellani et al (CCM 2013) compared the amplitude (Edi peak) of the Edi waveform to the measured work of breathing (Pmusc) in 10 adult patients on mechanical ventilation at three levels of assist during both PSV and NAVA. Although the Edi/Pmusc ratio (an index of “neuro-mechanical coupling”) was found to be variable between patients, within a patient, the ratio was constant for different modes and levels of assist. The authors concluded that the Edi was a valid index of global inspiratory muscle force, which confirms the findings of Beck et al from 2001 (Beck AJRCCM 2001).
Neuro-ventilatory efficiency and weaning: From University of Göttingen Medical School, Barwing et al (CC 2013) used the EAdi (combined with VT) as a monitoring parameter in eighteen adult patients that were having difficulty with weaning from the respirator. They performed a 30 min spontaneous breathing trial (SBT) with t-piece and 90% FIO2 and found a higher EAdipk (~26 mV) in the failure group, compared to the success group (13 mV). The neuro-ventilatory efficiency (NVE), calculated as ml/mV, was significantly lower in the failure group, compared to the success group. These findings confirm the results of two previous studies examining Edi and NVE as predictors of weaning success and failure (Liu CC 2012; Dres ICM 2012).
Neuro-ventilatory efficiency and weaning: Rozé et al, in The British Journal of Anesthesia (2013), also reported ventilatory and Edi parameters in 12 adult patients, undergoing daily SBTs (with PSV = 7 cm H2O, ZEEP). If patients failed the 30-min SBT, they were placed on NAVA ventilation (NAVA level set to 60% of Edipk during SBT), and the SBT was repeated the subsequent day. The process was continued until successful weaning was achieved. Their analysis included the (daily) increase in Edi and the drop in NVE when patients were switched from NAVA to SBT. Edi increased by equal amounts when switched from NAVA to SBT, regardless of success or failure, however, the drop in NVE was less for the success group. Interestingly, looking at the change in Vt from NAVA to the SBT, Vt could be maintained in the success group, whereas it dropped significantly in the failure group.
Edi and tidal volume matching: Chiew et al (Biomed Eng Online 2013) studied the relationship between the integrated Edi and VT, the so-called “Range90” index, during three different levels of non-invasive NAVA (NIV-NAVA) in 12 adult patients. A low Range90 index is suggestive of better “matching” between patient respiratory drive and delivery of assist. The NAVA level was set to the same peak pressure as during clinical PSV prior to the study (NAVA100), to 50% less (NAVA50) and 50% more (NAVA150). Globally, NAVA50 was found to have the best matching of Edi and VT (albeit only in 7 of the 12 patients). The authors also stated however, that NAVA level settings, based on their findings, are patient specific.
NAVA in prolonged weaning: In thirteen tracheotomised patients with prolonged weaning, Vagheggini G et al (Respir Med 2013) compared the physiological response to four different levels of PSV and NAVA. As the assist increased, the peak Edi decreased in both modes, however VT in PSV increased from 4.5 ml/kg to >6 ml/kg, whereas in NAVA, the VT at the highest assist level was 5 ml/kg. Neural respiratory rate did not change during different NAVA levels, but decreased with increasing PSV. Ineffective triggering was the same in both modes.
Note: These findings (NAVA reduces risk of overdistension by down-regulation of Edi) confirm those of 14 other studies (e.g. Colombo 2008; Brander 2009; Terzi 2011; and others).
Note: 17 adult studies (in 240 patients) show mean Vt values of 6.5ml/kg (range 5.9-9.9 ml/kg) on NAVA (mean breathing frequency is 25 bpm, range 18-30). In 14 infant studies, mean Vt was 6.4 ml/kg on NAVA (range 3-8.7 ml/kg) with a mean breathing frequency of 46 bpm (range 35-59).
Edi values in neonates: In the pediatric and neonatal literature, Stein and colleagues (J Perinatol 2013) were the first to publish Edi data in non-ventilated preterm neonates (n=17) (only highflow nasal cannula, nasal cannula or room air). Edi was collected weekly, up to 10 weeks. The average Edi peak was 10.8 uV (range 3.8 – 18.7) and the average Edi min was 2.8 uV (range 0.8-7.6) and did not change with postnatal maturation. No adverse events were reported with Edi catheter placement (similar to 6 other studies that specifically evaluated this, eg. Barwing, ICM 2009 or Duyndam, Nurs Crit Care 2013).
NAVA in neonatal RDS: In a Chinese study (Zhongguo Dang Dai Er Ke Za Zhi. 2013), Chen et al studied 10 preterm neonates with RDS, and compared NAVA to SIMV (1 hour each). They showed improved patient-ventilator interaction, with lower PIP, lower respiratory rate, lower Edi and lower work of breathing with NAVA.
NAVA in PICU (invasive and non-invasive): Improved patient-ventilator interaction with NAVA was also found in two separate papers by Vignaux et al (PCCM 2013a, PCCM 2013b) in pediatric patients undergoing invasive (19 infants) and non-invasive (6 infants) ventilation. Extensive manual analysis was performed on the airway pressure and Edi waveforms in these studies to reveal the asynchronies (wasted efforts, auto-triggering) and dys-synchronies (trigger and cycling-off delays).
Note: Interestingly, as of the end of 2013, 24 studies (PUBMED) in 329 patients of all ages have shown that NAVA improves synchrony compared to conventional ventilation modes. In the 17 studies (224 patients) that reported an Asynchrony Index, asynchrony was reduced with NAVA (26 to 5%, p<0.001). 19 studies in 301 patients of all ages report improved or equivalent physiological parameters.
NeuroSync index for patient-ventilator interaction: As an alternative to tedious and time-consuming (limiting the time periods for reasonable analysis), Sinderby et al, in Critical Care (2013), described an automated method to use the EAdi waveform in detecting and quantifying poor patient-ventilator interaction in adult patients on PSV. They described algorithms and a “NeuroSync Index” which could quantify patient-ventilator interaction, and could separate “asynchrony” from “dys-synchrony”. The algorithms reported were standardized and correlated well with manual analysis.
NAVA in Pediatric ARDS and outcomes: Piastra et al (J Crit Care 2013) performed a nested study to compare the clinical outcomes in children ventilated either with PSV (n=20) or NAVA (n=10) after a period of HFOV for severe ARDS. From HFOV, NAVA showed less of an increase in HR and blood pressure, showed an improved COMFORT score, lower PIP and PaCO2, and less duration on ventilation, than PSV.
Bellani G, Mauri T, Coppadoro A, Grasselli G, Patroniti N, Spadaro S, Sala V, Foti G, Pesenti A. Estimation of Patient’s Inspiratory Effort From the Electrical Activity of the Diaphragm. Crit Care Med. 2013 Jun;41(6):1483-91
Barwing J, Pedroni C, Olgemöller U, Quintel M, Moerer O. Electrical activity of the diaphragm (EAdi) as a monitoring parameter in difficult weaning from respirator: a pilot study. Crit Care. 2013 Aug 28;17(4):R182
Liu L, Liu H, Yang Y, Huang Y, Liu S, Beck J, Slutsky AS, Sinderby C, Qiu H. Neuro-ventilatory efficiency and extubation readiness in critically ill patients. Crit Care. 2012 Jul 31;16(4):R143. [Epub ahead of print]
Dres M, Schmidt M, Ferre A, Mayaux J, Similowski T, Demoule A. Diaphragm electromyographic activity as a predictor of weaning failure. Intensive Care Med. 2012 Dec;38(12):2017-25
Rozé H, Repusseau B, Perrier V, Germain A, Séramondi R, Dewitte A, Fleureau C, Ouattara A.Neuro-ventilatory efficiency during weaning from mechanical ventilation using neurally adjusted ventilatory assist. Br J Anaesth. 2013 Dec;111(6):955-60
Blankman P, Hasan D, van Mourik MS, Gommers D. Ventilation distribution measured with EIT at varying levels of pressure support and Neurally Adjusted Ventilatory Assist in patients with ALI. Intensive Care Med. 2013 Jun;39(6):1057-62
Chiew YS, Chase JG, Lambermont B, Roeseler J, Pretty C, Bialais E, Sottiaux T, Desaive T Effects of Neurally Adjusted Ventilatory Assist (NAVA) levels in non-invasive ventilated patients: titrating NAVA levels with electric diaphragmatic activity and tidal volume matching. Biomed Eng Online. 2013 Jul 2;12:61.
Vaschetto R, Cammarota G, Colombo D, Longhini F, Grossi F, Giovanniello A, Corte FD, Navalesi P. Effects of Propofol on Patient-Ventilator Synchrony and Interaction During Pressure Support Ventilation and Neurally Adjusted Ventilatory Assist. Crit Care Med. 2013 Aug 26. [Epub ahead of print]
Vagheggini G, Mazzoleni S, Vlad Panait E, Navalesi P, Ambrosino N. Physiologic response to various levels of pressure support and NAVA in prolonged weaning. Respir Med. 2013 Nov;107(11):1748-54
Colombo D, Cammarota G, Bergamaschi V, De Lucia M, Corte FD, Navalesi P. Physiologic response to varying levels of pressure support and neurally adjusted ventilatory assist in patients with acute respiratory failure. Intensive Care Med. 2008 Nov;34(11):2010-8
Brander L, Leong-Poi H, Beck J, Brunet F, Hutchison SJ, Slutsky AS, Sinderby C. Titration and Implementation of Neurally Adjusted Ventilatory Assist in Critically Ill Patients. Chest. 2009 Mar;135(3):695-703
Terzi N, Pelieu I, Guittet L, Ramakers M, Seguin A, Daubin C, Charbonneau P, du Cheyron D, Lofaso F. Neurally adjusted ventilatory assist in patients recovering spontaneous breathing after acute respiratory distress syndrome: physiological evaluation. Crit Care Med. 2010 Sep;38(9):1830-7
Stein H, Hall R, Davis K, White DB. Electrical activity of the diaphragm (Edi) values and Edi catheter placement in non-ventilated preterm neonates. J Perinatol. 2013 Sep;33(9):707-11
Chen Z, Luo F, Ma XL, Lin HJ, Shi LP, DU LZ. Application of neurally adjusted ventilatory assist in preterm infants with respiratory distress syndrome]. Zhongguo Dang Dai Er Ke Za Zhi. 2013 Sep;15(9):709-12
Vignaux L, Grazioli S, Piquilloud L, Bochaton N, Karam O, Jaecklin T, Levy-jamet Y, Tourneux P, Jolliet P, Rimensberger P. Optimizing patient ventilator synchrony during invasive ventilator assist in children and infants remains a difficult task. Pediatr Crit Care Med. 2013 Sep;14(7):e316-25
Vignaux L, Grazioli S, Piquilloud L, Bochaton N, Karam O, Jaecklin T, Levy-jamet Y, Tourneux P, Jolliet P, Rimensberger P. Patient-ventilator asynchrony during non-invasive pressure support ventilation and neurally adjusted ventilatory assist in infants and children. Pediatr Crit Care Med. 2013 Oct;14(8):e357-64
Sinderby C, Liu S, Colombo D, Camarotta G, Slutsky AS, Navalesi P, Beck J. An automated and standardized neural index to quantify patient-ventilator interaction. Crit Care. In Press Oct 2013
Piastra M, De Luca D, Costa R, Pizza A, De Sanctis R, Marzano L, Biasucci D, Visconti F, Conti G. Neurally adjusted ventilatory assist vs pressure support ventilation in infants recovering from severe acute respiratory distress syndrome: Nested study. J Crit Care. 2013 Oct 24. [Epub ahead of print]
Case reports (n=3)
Use of Edi for detecting Congenital Central Hypoventilation Syndrome: Both Rahmani et al (J Coll Physicians Surg Pak) and Szcapa et al demonstrated the use of monitoring Edi as a diagnostic tool in newborn infants suspected of having Congenital Central Hypoventilation Syndrome (CCHS), also known as “Ondine’s Curse”. In both cases, the infants had recurring hypoventilation and oxygen desaturation; they were admitted to the NICU and were intubated and mechanically ventilated. The Edi was measured in both children, and was found to be absent during sleep (and hypercapnia observed in the Sczapa study). Both centers subsequently performed genetic testing and confirmed CCHS.
Interference with Edi: Somers et al (Minerva Anesthesiol) reported a technical note, where electrical equipment (intra-aortic balloon catheter, a pacemaker and a heating device) could interfere with the Edi signal in the ICU. The study demonstrated the importance of catheter positioning procedures. One of the interfering devices has since been taken off the market. Note that despite this single case of report of pacemaker-related problems, the use of pacemaker during measurements of Edi/NAVA has previously been reported as non-problematic in other studies.
Rahmani A, Ur Rehman N, Chedid F. Neurally adjusted ventilatory assist (NAVA) mode as an adjunct diagnostic tool in congenital central hypoventilation syndrome. J Coll Physicians Surg Pak. 2013 Feb;23(2):154-6
Szcapa T, Beck J, et al. Monitoring Diaphragm Electrical Activity and the Detection of Congenital Central Hypoventilation Syndrome in a Newborn. J Perinatology, Nov;33(11):905-7.
Somers Y, Verbrugghe W, Jorens PG. Mechanical and electrical equipment interference provokes a misleading Neurally Adjusted Ventilatory Assist (NAVA) EAdi signal. A technical note. Minerva Anestesiol. 2013 Jul 1. [Epub ahead of print]
Letters and editorials (*) (n=10)
Moss KS. Neurally adjusted ventilatory assist: insufficient evidence of broad clinical outcomes. Respir Care. 2013 May;58(5):884-5
*Marini JJ. Monitoring breathing effort: A work in progress. CCM June 2013
*Gama de Abreu M, Belda FJ.Neurally adjusted ventilatory assist: letting the respiratory center take over control of ventilation.Intensive Care Med. 2013 Aug;39(8):1481-3.
*Tobin MJ. Probing with the ventilator. Crit Care. 2013 Oct 3;17(5):198.
*Ramet J, De Dooy J. Patient-ventilator asynchrony during noninvasive pressure support ventilation and neurally adjusted ventilatory assist in infants and children*.Pediatr Crit Care Med. 2013 Sep;14(7):728-9
*Piquilloud L, Jolliet P, Revelly JP. Automated detection of patient-ventilator asynchrony: new tool or new toy? Crit Care. 2013 Nov 20;17(6):1015. [Epub ahead of print]
Esquinas AM. Neurally Adjusted Ventilatory Assist vs Pressure Support Ventilation During Noninvasive Mechanical Ventilation: Another Physiologic Evaluation to Consider? Chest. 2013 Apr 1;143(4):1181
Futier E, Jaber S, Constantin JM. Response to Dr. Esquinas. Chest. 2013 Apr;143(4):1181-2.
Sinderby C. Neurally adjusted ventilatory assist: insufficient evidence of broad clinical outcomes. Respir Care. 2013 Nov;58(11):e153-4
Moss KS. Neurally adjusted ventilatory assist: insufficient evidence of broad clinical outcomes–reply. Respir Care. 2013 Nov;58(11):e154-7
Reviews (n=7)
Ducharme-Crevier L, Du Pont-Thibodeau G, Emeriaud G Interest of monitoring diaphragmatic electrical activity in the pediatric intensive care unit. Crit Care Res Pract. 2013;2013:384210
Sinderby C, Beck J. Neurally Adjusted Ventilatory Assist (NAVA) in Non-Invasive Ventilation. Minerva Anestesiol. 2013 Apr 5. [Epub ahead of print]
Fan E, Villar J, Slutsky AS. Novel approaches to minimize ventilator-induced lung injury. BMC Med. 2013 Mar 28;11:85
Gilstrap D, Macintyre N. Patient Ventilator Interactions: Implications for Clinical Management. Am J Respir Crit Care Med. 2013 Sep 26. [Epub ahead of print]
A Skorko, D Hadfield, A Shah, P Hopkins. Advances in Ventilation: neurally adjusted ventilatory assist (NAVA).JICS 14(4): 317-323, 2013
Stein H, Firestone K. Application of neurally adjusted ventilatory assist in neonates. Semin Fetal Neonatal Med. 2013 Nov 13.Epub Ahead of Print
Oppersma E, Doorduin J, van der Heijden EH, van der Hoeven JG, Heunks LM. Noninvasive ventilation and the upper airway: should we pay more attention? Crit Care. 2013 Dec 5;17(6):245. [Epub ahead of print]