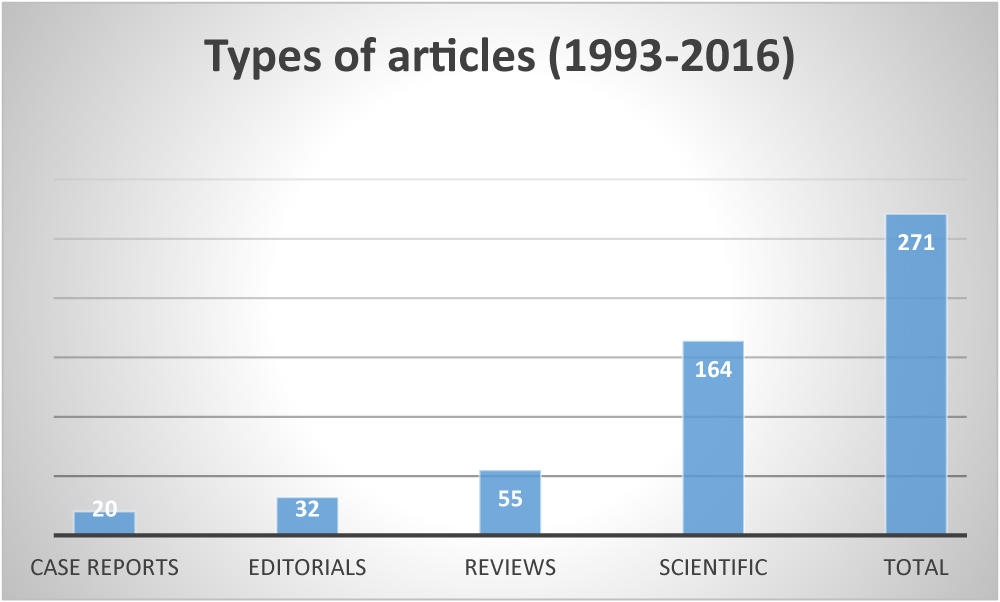
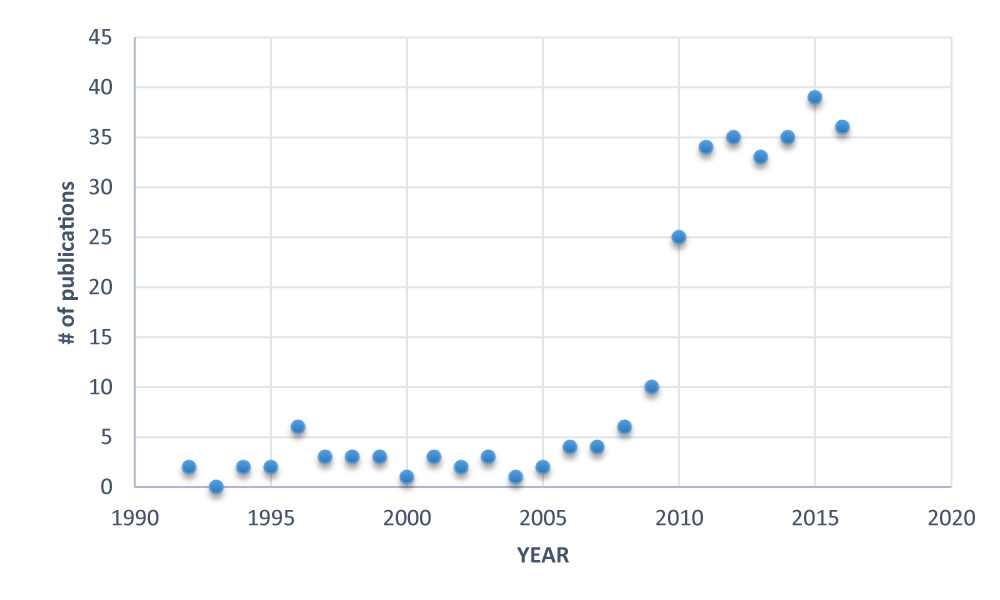
To date, 271 publications have described the science of NAVA and Edi monitoring.
In 2016, there were 36 publications on PUBMED, including 24 original scientific papers, 5 case reports, 3 editorials, and 4 reviews.
Studies in adults
Multi-Center Randomized Trial: NAVA vs. PSV
2016 marked the first publication of a multi-centre trial to evaluate clinical outcomes with NAVA in adult patients. Demoule et al (Intensive Care Med 42(11):1723-1732) included 128 intubated patients recovering from ARF (i.e. in the weaning phase); they were randomized to receive either PSV or NAVA, with a primary outcome variable being the probability of remaining in a partial ventilator mode throughout the first 48 hrs, without any return to assist control ventilation. They found equal probability in both groups, despite improved synchrony, improved comfort and less post-extubation NIV in the NAVA patients. An editorial accompanied this work (Navalesi, 42(11):1770-1771), as well as a commentary letter (Sinderby, Demoule, Similowski, Intensive Care Med, 2017).
NAVA during ECMO in ARDS
Mauri et al (Anesthesiology 125:159-167) studied eight spontaneously breathing ARDS patients undergoing venovenous ECMO. During both PSV and NAVA, they manipulated the ECMO gas flow (decreased from a defined baseline, 4 different levels) for 20-minute periods in each mode. With increasing gas flow, they observed reductions in all measured variables: Edi, P 0.1, transpulmonary pressure, tidal volume and airway pressure. Contrary to PSV, the assist levels increased during NAVA as gas flow was reduced (and Edi increased). The authors suggested that increasing the NAVA level would down-regulate the Edi further if lung-protection is the goal.
NAVA vs. PSV on Diaphragm Efficiency
The impact of prolonged assisted ventilation on diaphragmatic efficiency was evaluated by Di mussi et al (Critical Care, 20:1-12) for patients ventilated on NAVA versus PSV. Twenty five patients whom had received controlled mechanical ventilation for at least 72 hrs were randomized to receive either NAVA (n=13) or PSV (n=12) for a 48 hr period and neuromechanical efficiency (NME) and neuroventilatory efficiency (NVE) were measured 3 times (0, 24 and 48h) during a spontaneous breathing trial. NVE and NME were similar at baseline, but after 48 hours, the values were significantly higher in the NAVA group. The results imply better preservation of diaphragm function with NAVA. Edi peak values were on average higher during NAVA (~10 uV) compared to PSV (~6 uV).
Randomized Controlled Trial Protocol for NAVA vs. Conventional Ventilation
A protocol for a randomized controlled trial was published by Villar et al the “NAVIATOR” trial (Trials. 17:500-509). The investigators plan on recruiting 306 mechanically ventilated patients with acute respiratory failure. The inclusion criteria are: Patients ventilated less than 5 days, and who are expected to require prolonged mechanical ventilation for at least 72 more hours. Patients will be randomly assigned to either NAVA or conventional ventilation and the outcome will be evaluated based on ventilator-free days (defined as days alive and free of ventilation at day 28 after intubation.
NAVA with Helmet Interface
In 15 hypoxemic patients ventilated non-invasively after extubation, Cammarota et al (Anesthesiology 125(6): 1181-1189) studied 3 modes of ventilation delivered through two different “helmets” (i) PSV, (ii) NAVA and (iii) neural PSV (i.e. NAVA mode set with highest NAVA level, while limiting the upper pressure). Their outcomes included patient comfort, Edi, patient-ventilator interaction and blood gases. The two helmets (standard fixation straps vs. new helmet) were randomized, and then the 3 modes were randomized, and applied for 30 minutes each. Comfort score was significantly improved with both helmets from standard PS to NAVA to neural PS, and was accompanied by a decrease in Edi peak. Blood gases were similar for all ventilation periods. As per study design, the pressurization rate was fastest with neural PS. Synchrony was improved with NAVA and neural PS compared to pneumatic PS.
NAVA for Difficult to Wean COPD
In a randomized clinical trial, Kuo et al (International J of COPD 11: 945-951) studied 33 COPD patients with ventilator dependency (defined as >21 days in a weaning centre). They compared NAVA patients (n=14) to conventional ventilation (PSV or ACV, n=19) in terms of weaning outcome and asynchrony, in patients who had been ventilated for more than 21 days. Spontaneous breathing trials (PS of 8, PEEP 5) were performed every 24 hrs and if successful, patients were extubated to NIV. They confirmed previous reports, that the asynchrony index was lower in NAVA compared to conventional ventilation, and that the Edi helped to improve detection of asynchrony. Although not statistically significant, the authors claimed that the clinical outcomes (mortality and weaning outcomes) were improved with NAVA.
NIV-NAVA in COPD
In a study involving 40 patients with acute exacerbation of COPD, Wang et al (Zhonghua Yi Xue Za Zhi 15:96(42):3375-3378) studied the impact of non-invasive NAVA and NIV-PSV on synchrony and gas exchange. The authors report similar improvements in gas exchange with the two modes, but synchrony was improved with NIV-NAVA (shorter trigger delay, shorter cycling-off delay, less ineffective efforts and autotriggering and double triggering).
Edi Monitoring during Bronchodilator Therapy in COPD
Li et al (J Thoracic Dis 8(5):958-965) describe an exploratory study in 36 non-ventilated mild-to-moderate COPD subjects, where the Edi signal was used to evaluate the responsiveness to bronchodilator therapy. Half the patients (Group A) were randomized to receive placebo, Salbutamol, then Ipratropium, whereas the other half (Group B) received placebo, and reversed the order of Ipratropium and Salbutamol. Pulmonary function tests and Edi and dyspnea measurements were performed at the end of each period (15-30 min depending on the drug provided). Bronchodilators significantly improved the pulmonary function tests, reduced dyspnea, and the Edi signal, compared to placebo. The authors found that the ratio of minute ventilation to the Edi amplitude had the greatest sensitivity to detect bronchodilator efficacy. They concluded that neural respiratory drive seems to be a promising and sensitive index to evaluate the responsiveness to bronchodilators.
Edi-Based Measures for Outcome Evaluation
In a retrospective study, Bellani et al (Respir Care 61(4): 495-501) used a previously published index (ratio of inspiratory muscle pressure, Pmus and the electrical activity of the diaphragm, EAdi) and compared values of the index over time during an ICU stay. Inclusion was: (1) at least one measurement of Pmus/EAdi during the first 48h of transition from controlled ventilation to spontaneous modes, and (2) at least on measurement in the last 48 h before extubation. Forty-one adult (mean age 60 yrs) subjects were included, with a mean duration of controlled ventilation of 4 days, and duration of deep sedation of 6 days. The mean Pmus/EAdi was 1.04 cm H2O per uV, similar to the values obtained in their validation paper in 10 ventilated ICU patients (Bellani et al. Critical Care Med 41(6):1483-1491, 2013). No trends were observed in Pmus/EAdi over the course of ICU stay, and no differences in clinical outcome were correlated to the index.
Patient-Ventilator Interaction during Dexmedetomidine vs. Propofol
In a multi-centre, prospective, open label randomized clinical trial, Conti et al (Critical Care 20:206-214) studied patient-ventilator interaction with two types of sedatives: Dexmedetomidine (Dex) and standard propofol sedation; the comparison was made at similar RASS scores. Twenty adult ICU patients who had failed their first weaning trial were included. While ventilated in the PS mode, the Edi and ventilator signals were recorded for 10 minutes at varying intervals over a 24-hr period. The asynchrony index was found to be lower for Dex patients than with propofol from 2 hours onwards, reaching significance at 12 hrs. At similar levels of PSV, the two groups had no significant differences for time in synchrony, tidal volume, respiratory rate and blood gases. Edi peak tended to be lower with propofol (~10 uV), compared to Dex (~16 uV) but this was not significant. The authors concluded that the use of Dex sedation may offer an advantage in terms of patient-ventilator synchrony.
Partial Neuromuscular Blockade during NAVA
Doorduin et al (AJRCCM October 2016, Published ahead of print), performed a proof-of-concept study aiming to show that a low dose of rocuronium (partial neuromuscular blockade) facilitates lung protective ventilation during spontaneous breathing, by allowing a reduction in muscular activity. In 10 sedated ARDS patients with lung injury and tidal volume >8 ml/kg, rocuronium was administered to target a tidal volume of 6 ml/kg during NAVA. Respiratory and hemodynamic measures were taken while patients were ventilated with either PSV or NAVA (2 hours each mode) under continuous infusion of rocuronium. They demonstrated significant reductions in tidal volume, transpulmonary pressure and Edi, however, with increased hemodynamic consequences (mean arterial pressure and heart rate increased).
Systematic Review of NIV-NAVA
In a systematic review and meta-analysis in adults ventilated non-invasively with NAVA, Sehgal et al (Intensive Care Med 42(11):1813-1815) provide Forest plots of the mean difference of the asynchrony index between PSV and NAVA. This was a nice evidence-based summary showing the improved synchrony with NIV-NAVA, with a 3.4 times risk of asynchrony for those ventilated in NIV-PSV.
Case reports or “letter to the Editor” in adults
- A case report by Sangha and Whitacre (J Intensive Care Med. 32(2):170-173) shows the importance of Edi monitoring to detect ventilator auto-triggering.
- Another case report by Goto et al (J Intensive Care. 4: 26-32) described an ARDS patient who was ventilated with NAVA after failing weaning with (asynchronous) conventional ventilation. The authors described improved gas exchange and lung aeration in dorsal and mid-dorsal regions with NAVA (using EIT).
- In a “Letter to the Editor”, Schellekens and Heunks (Intensive Care Med 42:633-634) respond to a paper reporting inappropriate NAVA catheter placement complicated by hydropneumothorax. The letter states that the authors should have used additional criteria, such as retrocardial ECG pattern, to verify the position.
- The first Indian case report by Baldi et al (Indian Journal of Crit Care Med 20:364-367) was published and described a 55-yr old patient with ARDS and difficult weaning (>30 days invasive conventional ventilation), believed to be a result of poor patient-ventilator interaction. The patient was placed on NAVA and gradually weaned and extubated 2 days later.
Studies in infants
Randomized Trial of NAVA vs. Conventional Ventilation In Preterm Infants
Kallio et al (Eur J Pediatrics 175:1175-1183) performed a randomized controlled trial in 60 preterm infants (28-36+6 weeks GA with at least 4 hrs invasive ventilation). Babies were randomized to either NAVA or conventional ventilation, and the primary outcome was duration of invasive ventilation. The extubation criteria were: FIO2<0.4, PIP<16 cm H2O, satisfactory rate and tidal volume with lowering of support. The investigators found no difference in the median times to extubation or NICU stay between the 2 groups. Despite similar tidal volumes, the patients in the NAVA group had lower pressures than in the conventional arm. 60% of the NAVA group had reached extubation criteria (<16 cm H2O PIP) during the first data collection period, but they were not extubated for clinical reasons. The amount of opiates did not differ between groups. The authors recommend that new extubation criteria are required for the NAVA mode.
NAVA in BPD
In a retrospective study, Jung et al (Ped Crit Care 17(12): 1142-1146) examined ventilatory data from 29 preterm infants (median GA 25 weeks, BW 680g) with bronchopulmonary dysplasia (ventilated invasively at least 4 weeks and respiratory severity score >4) as they were transitioned from SIMV to NAVA, and followed over 24 hrs. They found significantly lower PIP, mean airway pressure, Edi and work of breathing during NAVA, compared to SIMV. As well, there was a significant improvement in arterial blood gases and less oxygenation requirements, over a 24-hr period of NAVA. No adverse effects were observed during NAVA ventilation, which as a median value, lasted 18.5 days after the transition from SIMV.
NAVA and NIV-NAVA Titration in Preterm Infants
The recent paper by LoVerde, Firestone, and Stein (J Perinatology. 36(12):1097-1100) contradicts the wide-held assumption that the respiratory control system in preterms is not appropriate for NAVA. In a group of fifteen premature infants (mean birth weight 950g; gestational age 26.8 weeks), the authors showed down-regulation of respiratory drive (Edi) with increasing levels of NAVA, thereby limiting increases in tidal volume and peak inspiratory pressure. This physiological response was demonstrated before (invasive NAVA) and after extubation (non-invasive NAVA). The authors found that the “breakpoint” during the NAVA level titration, occurred at slightly higher pressures (~ 5 cm H2O) during NIV-NAVA.
NIV-NAVA in Pediatric Patients
Chidini et al (Ped Crit Care Med 17:e487-e495) studied 18 children with acute respiratory failure needing non-invasive ventilation, upon admission to the PICU. All consecutively-admitted patients were eligible if they had P/F ratio <300 and at least two of the following. High respiratory rate, use of accessory muscles, and paradoxical abdominal motion, and need for a feeding tube and an indwelling arterial line. Children underwent either NIV-PS or NIV-NAVA for 60 minutes (randomized), and then switched to the other mode for an additional 60 minutes; a full-face mask was used. The primary outcome was the asynchrony index, which was significantly lower during NIV-NAVA. All types of asynchrony measures were lower with NIV-NAVA, but mainly ineffective efforts. Sedation use was similar for the two periods, as were the blood gases.
NAVA vs. Conventional Ventilation in Post-Cardiac Surgery and Cerebral Blood Flow
Zhu et al (Pediatr Cardiology 37:1064-1071) evaluated cerebral blood flow and arterial oxygenation in 21 pediatric patients (median age 10 months, weight 7.5 kg) after Bidirectional Superior Cavopulmonary Anastomosis (BCPA). After cardiac surgery, the following interventions were studied: (i) PC before awake from anesthesia at lower (10 ml/kg) and higher tidal volume (15 ml/kg); (ii) 2 minutes of CPAP to establish a high Edi tolerated; (iii) random assignment of PSV or NAVA, at low and high levels of assist. (*Note the original n = 23 was reduced to n = 21 because two infants had bilateral diaphragm paralysis post-surgery.). The main differences between NAVA and PSV at high levels of assist were higher VT, PIP, and MAP in PSV. Blood gases were improved with NAVA at both the low and high levels of assist, compared to PSV. Increasing NAVA levels did not alter VT (~10 ml/kg) (different from PSV where VT increased at higher assist). Cerebral blood flow was more optimal during NAVA.
NAVA vs. Conventional ventilation and Hemodynamics Post-Cardiac Surgery
Liet et al (BMC Pediatrics 16:180-186) examined the physiological (mainly hemodynamic) effects of NAVA versus conventional ventilation (a combination of volume control and PSV) in patients who had undergone cardiac surgery. Six infants (mean age 7.8 months) were studied for 30 minutes (data recorded in the last 10 min of each period), either on NAVA or conventional ventilation, while attempting to maintain minute volumes constant during both modes. Four of the infants had an already initial low central venous oxygenation, tended to increase their cardiac index with NAVA compared to conventional. For the group of six infants, the mean cardiac index did not change significantly; there were no differences in tidal volume, minute ventilation or pH. PIP was lower with NAVA. The authors concluded that their pilot study suggests that NAVA could have a beneficial effect on hemodynamics in children.
Edi Monitoring during Different Feeding Methods (FEAdi Trial)
The role of feeding methods (slow feed vs. bolus feed) on neural breathing pattern was recently described by Ng et al (Early Human Development 101:33-37). In a prospective randomized, cross-over trial, 10 non-ventilated infants (mean birth weight 1050g, study weight 1480g, study age 27.5 days) were fed by bolus feed or slow infusion feed over 90 min. There was a high variability in terms of response to feeding methods (Edi min, Edi pk, neural Respiratory rate, central apnea), with no group mean differences for the two feeding methods. The authors concluded that feeding method does not affect breathing pattern, and that in particular, a bolus feed does not seem to induce increased central apnea.
Efficient Post-Extubation Support with NIV-NAVA in Preterms
In a retrospective study in 24 newly-extubated preterm neonates (mean birth weight 814 g), Colaizy et al describe the capacity of NIV-NAVA to provide efficient ventilator support, as defined by a reduction in PCO2, with an increase in NAVA levels (Perinatol. 2016 Dec 5. [Epub ahead of print]). In 83% of the babies, an increase in the NAVA level demonstrated a decrease in PCO2 (“responders”), while in the remaining patients, the increase in assist had no impact (“non-responders”). There were no differences between groups in term of age, weight or days since extubation. The median decrease in PCO2 for the entire cohort was 4 mm Hg, and was 5 mm Hg for the responders. Of note, the responders had higher levels of NAVA (1.4 vs. 0.6 cm H2O/uV). The authors concluded thatNIV-NAVA can produce efficient and synchronized support after extubation, as measured by PCO2.
Case report in infants
- From Roosens et al (Ped Pulm 51:E37-E39): after admission to the NICU for neonatal resuscitation, a 2.5 kg baby (one of twins) was sedated and ventilated for 6 days with conventional ventilation, and extubated to CPAP, which was not satisfactory support. X-ray revealed elevation of the right hemidiaphragm: the infant had unilateral diaphragm paralysis. The infant was switched to non-invasive NAVA and ventilated with a nasal mask, and ventilated with acceptable Edi values (6-20 uV) and NAVA level (1.5. cm H2O/uV). CO2 and feeding tolerance improved. The diaphragm paralysis recovered after 3 months and the child was discharged home without additional support.
- Cosi et al (Pediatrics. Nov;138(5)) report a case of 4-month-old infant with asphyxiating thoracic dystrophy and respiratory failure successfully ventilated with NAVA. The investigators noted marked improvement in feeding tolerance with NAVA, allowing for weight gain and eligibility for thoracic surgery.
One editorial appeared in 2016 in relation to NAVA in Children (Piastra and Conti. Minerva Anestesiol.82(8):818-20).
Studies in animals
Feasibility of NAVA during Anesthesia
In an animal model (juvenile pigs ~27kg), the feasibility of NAVA was tested during sedation and anesthesia (Campoccia Jalde et al, Eur J of Anesthesiology, 33:283-291). During NAVA ventilation, animals were receiving either Sevoflurane or Propofol, with or without remifentanil, each for 15 min with extra washout periods. Blood gases were collected at the end of each period, as well as neuroventilatory (NVE) and neuromechanical efficiency (NME) measures. The last 5 min of the ventilator data was analyzed off-line. The Edi was well-preserved with both sedation and anesthesia. However, they found a lower Edi value during Sevoflurane, resulting in lower tidal volume and delivered pressure, compared to Propofol. Variability in tidal volume was also preserved with Sevoflurane. NME and NVE were higher with Sevoflurane. The authors suggest that NAVA could be used in the operating room.
Role of NAVA and PSV on Gastroesophageal Reflux
Cantin et al (PLOSone 11(1):e0146742) examined the role of non-invasive positive pressure ventilation NIPPV, using either nasal PSV or nasal NAVA, on gastroesophageal reflux in non-sedated spontaneously breathing newborn lambs (~4.6 kg). Gastro-esophageal reflux, esophageal insufflations, states of alertness, and ventilator and breathing pattern variables were continuously and wirelessly recorded during 3 consecutive days, where the animals were ventilated for 6 hours, with either nasal NAVA, nasal PSV, or no nasal ventilation (control). The main finding was similar reductions (inhibition) in gastroesophageal reflux, and similar insufflations into the esophagus in both modes, compared to control conditions. These findings are similar to what the investigators previously reported for nasal CPAP.
Continuous NAVA and Lung Protection
Brander et al (Respir Physiol Neurobiol. Mar;237:57-67) performed a study using Continuous NAVA (Edi controls pressure continuously and provides neutrally adjusted PEEP) in rabbits (3-4 kg) with acute lung injury. Using CT imaging, the authors demonstrated in an open-chest model (hence, respiratory muscles disabled) that lung protective reflexes are integrated during continuous NAVA as evidenced by improved aeration and prevention of over-distension during titrations of the NAVA level. This was confirmed to be vagally mediated, as vagotomy resulted in a lack of expiratory Edi (no control of PEEP), and cyclic lung collapse. With NIV-NAVA, removal of the expiratory assist was compensated by increased tonic Edi and PEEP, or by increased upper airway braking of expiratory flow.
Expiratory Edi and Lung Aeration in ARDS Animal Model
In 10 pigs with mild ARDS (target P/F 250), Pelligrinni et al (Am J Resp Crit Care Med, Dec 6, Epub ahead of print) report the role of expiratory Edi on lung aeration. CPAP was gradually reduced from 15 cm H2O to zero, in steps of 3 cm H2O, and dynamic CT scan images, and the procedure was also repeated during paralysis in 5 of the animals. The investigators found a linear correlation between expiratory Edi and transdiaphragmatic pressure (Pdi), the correlation being stronger at lower lung volumes. Edi and Pdi during expiration was elevated with decreasing CPAP. Atelectasis was observed during paralysis and mechanical eventilation at low PEEP levels, which was not observed during spontaneous breathing. The authors concluded that they demonstrate a central role of the diaphragm during breath-by-breath maintenance of alveolar inflation and protection against lung collapse.
Reviews
Four reviews which discuss NAVA and NIV-NAVA were published (one in adults, 3 in neonates):
- Gilstrap and Davies. Clin Chest Med. 2016 Dec;37(4):669-681
- Alexiou et al. Semin Fetal Neonatal Med. Jun;21(3):174-80
- Stein, Beck, and Dunn. Semin Fetal Neonatal Med. 2016 Jun;21(3):154-61.
- Firestone, Beck, and Stein. Clin Perinatol. 2016 Dec;43(4):707-724
