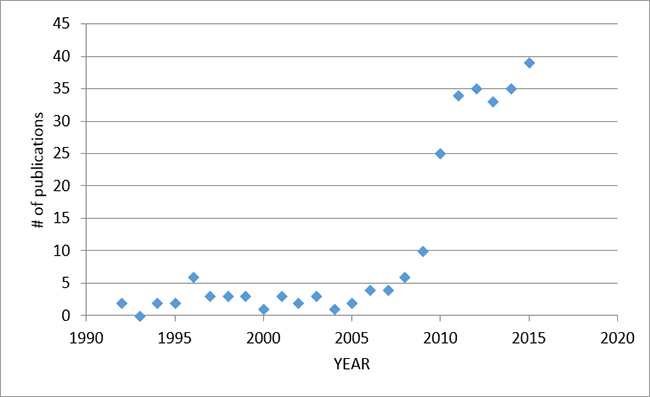
In 2015, there were 39 publications on PUBMED, including 24 original scientific papers, 4 case reports, 3 editorials, and 8 reviews.
Studies in adults
24-hrs evaluation of patient-ventilator interaction during NAVA vs. PSV
In 30 difficult to wean adult patients (mean duration of ventilation 33 days), Younis et al (BMC Anesthesiology) collected ventilator and physiological data over two 23-hr periods (either during NAVA or PSV), followed by a cross-over to the other mode. 80% of the patients underwent the PSV mode first. They found a lower total number of asynchronies and lower asynchrony index in the NAVA mode, as well as increased variability of tidal volume and oxygenation parameters.
This manuscript was accompanied by an editorial by Kacmarek et al (BMC Anesthesiology), who suggested that in most circumstances, it is suitable to utilize proportional modes of assist.
Neurally-triggered pressure support in patients with COPD
Using the Servoi ventilator set in the NAVA mode with the highest possible NAVA level, Liu et al (Critical Care) used adjustments in upper pressure limits to mimic neurally-triggered pressure support (PSN). At different levels of PEEP, they compared patient-ventilator interaction and physiological variables during PSN and during pneumatically-controlled pressure support (PSP) in 12 COPD patients with known intrinsic PEEP. The asynchrony index was lower with PSN compared to PSP, and remained low with PSN, even at zero PEEP. The impact of the improved synchrony was reduced pre-trigger and inspiratory mechanical efforts (evaluated by esophageal balloon). During PSP set at “optimal PEEP” (PEEP set to 80% of intrinsic PEEP), the effort to trigger was reduced during PSN, even when PEEP was zero. The authors concluded that PSN abolishes the need for extrinsic PEEP in COPD patients (for the purpose of triggering effort).
Lung-Distending Pressure during NAVA in ARDS
Doorduin et al (Critical Care Medicine) studied 12 patients with mild to moderate ARDS while breathing with three different ventilation modes (Pressure Control (PCV), Pressure support (PSV), or NAVA). The aim was to compare tidal volume and lung-distending pressure (transpulmonary pressure) between modes. The authors found that as patients were given more “freedom” to control the level of assist (PCV to PSV to NAVA), they were able to maintain lung protective ventilation with NAVA (mean chosen VT ~6.0 ml/kg), with the added benefits of improved respiratory variability and improved patient-ventilator interaction.
Patient vs. Ventilator Contribution to Tidal Volume
In an attempt to reproduce the PVBC concept in humans (“patient-ventilator breath contribution” index, Grasselli et al 2012 ICM), Liu et al (Critical Care) studied 12 intubated patients with acute respiratory failure during NAVA ventilation at different NAVA levels. At each NAVA level, for one breath, the assist was removed. The authors then calculated a ratio of tidal volume per Edi (VTinsp/Edipk) for this non-assisted breath, as well as for the preceding assisted breath(s). By dividing the Vtinsp/Edipk of the unassisted breath by the same ratio of the assisted breath, it was shown that this PVBC index was correlated to the gold standard index of esophageal pressure to transpulmonary pressure (Pes/PL). Squaring the PVBC increased this correlation to Pes/PL. Even further improvements were found if the average of five assisted breaths was used in the calculation of PVBC, and if the Edipk values were reproducible (30% error acceptable).
NAVA vs. PAV
In Critical Care, Schmidt et al compared PSV to two modes of proportional assist, NAVA and proportional assist ventilation (PAV), in 16 intubated patients (mainly ARDS and pneumonia). The main physiological outcomes included ventilation variables (and their variability), Edi, blood gases, and patient-ventilator asynchronies. The intervention was three different levels of support (initial 6-8 ml/kg, 50% lower, and 50% higher assist). The authors found better patient-ventilator interaction with PAV and NAVA, as well as improved variability in tidal volume. The only significant differences between PAV and NAVA were better proportionality with NAVA, and more double triggering (albeit a small frequency of these events per minute). Compared to PSV, both NAVA and PAV limited over-distension when the assist was increased.
Mathematical Modelling of Respiratory Elastance during NAVA and PSV
In a PLoS ONE article, Chiew and colleagues obtained experimental data in 22 patients to validate a time-varying elastance model in spontaneously breathing patients, using two modes, NAVA and PSV. Time-varying elastance (Edrs) trajectories were mapped and found to be significantly different between the two modes. A positive Edrs value is to be expected for patients who are not spontaneously breathing (full assist), whereas a negative Edrs value is indicative of more contribution of patient effort (more negative pleural pressure).
Diaphragm Ultrasound and Edi in Mechanically Ventilated Patients
Goligher et al, in a unique study (ICM), investigated the feasibility, reproducibility, and validity of measuring diaphragm thickness with ultrasound in mechanically ventilated patients. In 96 patients on mechanical ventilation, and in 9 healthy subjects (breathing spontaneously with different maneuvers), diaphragm thickening (an indication of inspiratory effort) and diaphragm thickness (an indication of diaphragm atrophy) were measured and compared to Edi. Right hemi-diaphragm thickness measures were highly reproducible, whereas diaphragm thickening fraction was only moderately reproducible, but was correlated to Edi. Patients who had undergone mechanical ventilation with neuromuscular blockade had a lower inspiratory thickening fraction, compared to those patients who received only partial ventilator assist, and healthy subjects.
Respiratory Muscle Unloading during NAVA vs. PSV
In 11 adult patients recovering from acute respiratory failure, Carteaux et al (Crit Care Med) sought to find comparable levels of respiratory muscle unloading during PSV and NAVA. In a randomized fashion, patients were studied at nine different NAVA levels, and at five different PSV levels, and indices of muscle unloading were calculated at each. More specifically, to express the percentage of assistance in a comparable way between the two modes, the authors calculated a ratio to quantify the proportion of the total pressure that was assumed by the ventilator (the remainder being the patient’s contribution). They concluded that – in terms of respiratory muscle unloading – levels of NAVA between 0.5 and 2.5 cm H2O/uV were comparable to PS levels ranging from 7 to 25 Cm H2O.
Tidal Volume during NAVA Ventilation after Double Lung Transplant
In a letter to the editor of the American Journal of Respiratory and Critical Care Medicine, Rozé et al report in a group of post lung-transplant patients (n = 14 ) the spontaneously chosen tidal volume while breathing on NAVA. A group of non-transplanted patients (surgical patients failing routine SBTs) served as controls. The transplanted patients demonstrated tidal volumes ranging from 2.9-7.5 ml/kg (mean 5.3 ml/kg). When hypercapnia was considered, there was no difference in tidal volume: 4.8 (1.2) ml/kg in the hypercapnic group vs. 5.9 (1.2) ml/kg in the non-hypercapnic patients. The tidal volume in the control group was 6.5 (1.5) ml/kg and was significantly higher than in the transplanted patients. This is the first study to demonstrate that bilateral vagal denervation is not an exclusion for NAVA ventilation, in terms of the spontaneously chosen tidal volume.
Potential Cost Savings with NAVA in Adults
Hjelmgren et al (Therapeutic Advances in Resp Dis) conducted an economic evaluation of NAVA compared with PSV based on previous reports showing an indirect link between improved patient-ventilator synchrony and time on ventilation. The cost of Swedish ICU cost and NAVA costs were incorporated into the model. The authors found a 31% improvement in synchrony with NAVA for all studies published, and extrapolated a 1.7 days reduction in days on mechanical ventilation. This would theoretically correspond to a cost savings of US$ 7886.
Studies in Children
Monitoring Edi during High-Flow Nasal Cannula in Premature Infants
Regarding Edi monitoring during nasal HFNC, Nasef et al (Acta Pediatr) compared neural breathing pattern during nasal CPAP and nasal HFNC matched to target the same mean airway pressure, in ten preterm infants (<1500 g). They found that nasal HFNC was associated with higher Edi peak, and increased neural inspiratory time, compared to nasal CPAP. As well, they observed a discrepancy between the respiratory rate of the patient determined from the Edi, and the respiratory rate noted by readings from the plethysmograph.
NIV-NAVA Improves Patient-Ventilator Interaction in Children
In a physiological cross-over study by Ducharme-Crevier (Crit Care), NIV-NAVA was compared to conventional NIV (CPAP, PSV, or PCV), in 13 children admitted to the PICU for respiratory failure (interquartile age range 2-109 months), eight of which had pneumonia or bronchiolitis. The authors found that during conventional NIV, patients spent between 27-32 percent of the time in asynchrony, while it was only 8% of the time in NIV-NAVA. This was mainly a result of reduced trigger delay, reduced cycling-off delay and less ineffective efforts.
NIV-NAVA Improves Patient-Ventilator Interaction in Preterm Neonates
The group of Lee et al (Arch Dis Child Fetal Neonatal Ed) examined timing errors between the Edi and ventilator pressure in 15 premature infants (mean GA 27 weeks) during NIV-NAVA and NIV-PSV. Besides a reduced amount of ineffective efforts and reduced auto-triggering, the authors found shorter trigger delays, and shorter time “in excess” during NIV-NAVA compared to NIV-PSV. During NIV-NAVA, the Edi and peak inspiratory pressure were lower. The overall asynchrony index during NIV-PSV was 74% (compared to NIV-NAVA 20%).
Use of NAVA in Nordic PICUs for Treatment of Acute Lung Injury
This study by Jensen et al (Acta Anesthesiol Scand) used questionnaire responses from 18 large Nordic ICUs that treat children with ARDS. NAVA was used in 44% of the units. They also found that other ventilation treatment strategies (cuffed endotracheal tubes, use of ECMO, etc…) for pediatric ARDS in the Nordic countries are relatively uniform and largely in accordance with international practice.
The Effect of Caffeine of Neural Respiratory Drive
In 17 premature infants on various modes of ventilation, the Edi waveform was analyzed before and after administration of a loading dose of caffeine citrate. Parikka et al (Early Human Dev) demonstrated a reduced number of central apneas (5-10s), and increased Edi amplitude after caffeine.
Tonic Edi with and without assist in the PICU
In 52 children (median 10 months old; inter-quartile range 1-49 months), Edi was recorded for 1-hour intervals at four periods throughout the PICU stay (acute phase, pre-extubation phase, post extubation phase, and at PICU discharge). The authors quantified the tonic Edi, and found in children <1 yr old (n=28), that tonic Edi increased from the acute phase to PICU discharge, but because inspiratory Edi concomitantly increased, the Edi as a percentage of the inspiratory effort, actually decreased over the course of PICU stay. In most of the older patients, tonic Edi was negligible (<0.5 uV), but could exceed over 1 uV at some point during the stay, indicating that older children can exhibit some degree of tonic Edi. Bronchiolitis was the only independent variable associated significantly with tonic Edi.
Impact of Sedation on Edi in the PICU
In the PICU, 20 children weaning from analgesia and sedatives were included and Edi was measured. The intervention in this study by Amigoni et al ( ICM) was a bolus of propofol (1 mg/kg), and the outcome was the Edi waveform’s lowest value (and time to reach that value). The mean decrement in Edi was 32%, most patients requiring less than 2 minutes to reach the lowest Edi. Backup ventilation had to be initiated in 6 children after a mean time of 6 minutes from drug administration. The authors concluded that the Edi signals should be used to measure the degree of respiratory depression, in order to better titrate the dosage.
Reflex Down-Regulation of Edi with Increasing NAVA Levels in Neonates
In agreement with studies in adult patients and in animals, Firestone et al (Journal of Perinatology) demonstrated an appropriate reflex response (i.e. down-regulation of Edi) to increasing NAVA levels in 21 preterm newborns (9 with invasive NAVA, 12 with NIV-NAVA). In the NAVA group, the mean birth weight was 703 g (380-960g) and in the NIV-NAVA group, it was 835 g (490-1060 g). In both groups, the NAVA level was initially set to 0.5 cm H2 O/uV, and was then increased in steps of 0.5 every 3 min until a NAVA level of 4 cm H2O/uV. Initially, peak inspiratory pressure increased with increasing NAVA levels, but then reached a “breaking point” (BrP), where it no longer increased, despite increasing NAVA levels. This is due to the down-regulation of Edi (by up to 53% at the BrP). Tidal volume also “plateaued” at the BrP.
NIV-NAVA in Children after Cardiac Surgery
In younger children receiving NIV for respiratory support following cardiac surgery, Hoetekie et al (Respiratory Care) performed a cross-over study by randomizing babies (age range 1-22 weeks, and less than 5 kg) to either nasal CPAP or NIV-NAVA right after extubation. The peak Edi values during NIV-NAVA were significantly lower during NIV-NAVA, indicating more diaphragm unloading compared to nasal CPAP. Synchrony analysis was reported for NIV-NAVA, and showed (despite average leakage of 70%), 99% neural triggering (compared to 95% in the Vignaux (5) study), with a low inspiratory trigger delay.
NAVA and Weight Gain in Very Low Birth Weight Infants
In the Journal of Clinical Neonatology, Rahmani et al. performed a retrospective analysis on medical records and found the median weight gain for babies who were treated with NAVA was higher (30g/day) than conventional ventilation (13 g/day), despite the same average caloric intake. The authors proposed a model to predict cost savings and reduced LOS. They concluded that this was the first study to provide insight into the potential financial impact of implementing NAVA.
NAVA Before and After Extubation in Term Infants
Longhini et al (Minerva Pediatrica) analyzed physiological and ventilator variables in 10 term infants (mean weight 3 kg) breathing for 2 hrs while intubated on NAVA and then extubated to NIV-NAVA, with the same ventilator settings. The authors found no differences in terms of gas exchange or breathing pattern between the two ventilation periods. Of note, there were no differences in patient-ventilator interaction, sedation requirements, nor vital signs for invasive or NIV-NAVA.
Animal Studies
Neurally Adjusted PEEP in Animals
In rabbits faced with respiratory challenges (resistance, CO2 rebreathing, and acute lung injury), Liu et al (BMC Anesthesiol) described for the first time the concept of “Continuous NAVA” (cNAVA). cNAVA is a new respiratory support device where the Edi controls the delivery of assist continuously both during inspiration and during expiration. (This is different from the commercially available mode known as NAVA which is triggered and cycled-off by the Edi, and is limited to proportional assist on inspiration only, with a fixed PEEP). With cNAVA, if there is Edi during exhalation (“tonic Edi”), assist will be delivered in proportion, hence a “neurally adjusted PEEP”.
Case Reports
In 2015, case reports were published demonstrating the clinical use of Edi monitoring and NAVA in an adult patient with tetanus (Tane, Respiratory Care), in neonates undergoing treatment with albuterol (Snow, Advances in Neonatal Care), and in two children with pulmonary interstitial edema (Lee, Journal of Clinical neonatology). One article reported the misplacement of the NAVA catheter into the lung (van Kerckhoven), the latter which can be avoided if the appropriate steps are taken for catheter insertion and placement.
